Dental sealants block cavity-causing bacteria, plaque, and food particles from collecting in the deep grooves on the chewing surfaces of back teeth, so tooth decay cavities are less likely to start. Dental sealants create a thin barrier over the enamel of molars and premolars, sealing out debris where brushing and flossing struggle to reach.
Dental sealants are one of the most common preventive dentistry treatments. Dental sealants are placed by dentists or hygienists during a routine Dental Care visit. The dental sealant application is fast, painless, and uses a cured sealant material that bonds to enamel.
Table of Contents
What are dental sealants?

Dental sealants (Dental Sealants) are thin coatings painted onto the chewing surfaces of premolars and molars. These back teeth molars often have deep grooves, pits, and fissures where cavity-causing bacteria and food debris get trapped. Once the sealant material hardens, the coating becomes a pit and fissure barrier that helps protect your teeth.
What is the purpose of sealants?
Dental sealants do four practical things that matter for tooth decay prevention:
- Seal deep grooves. Sealants cover deep grooves so bacteria cannot colonize as easily, supporting microbial invasion prevention and bacteria colonization block.
- Reduce acid exposure. Fewer trapped food particles means fewer acids produced by bacteria, improving acid attack resistance and enamel demineralization shield.
- Lower cavity risk on chewing surfaces. The Centers for Disease Control and Prevention (CDC) states that sealants on back teeth prevent a large share of cavities on those surfaces.
- Support early cavity intervention in select cases. Some guidance notes sealants can be used over areas of early decay to help stop progression, which is a form of incipient lesion arrest when correctly indicated and monitored.
Where do sealants go?
Sealants are mainly used on the chewing surfaces of:
- Permanent molars and premolars (permanent molars premolars)
- Sometimes primary teeth (baby teeth) if deep grooves and high caries risk exist, which is common in Pediatric Dentistry planning
Treatment Details
What are dental sealants made of?
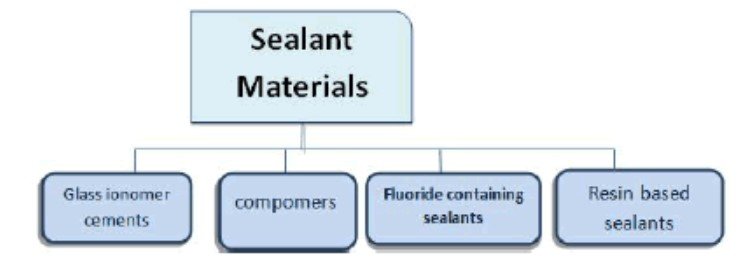
Dental sealants made for clinical use commonly fall into two categories:
- Resin-based sealants (Resin-based Sealants): Medical-grade resins that cure and harden into a protective resin application.
- Glass ionomer sealants (Glass Ionomer Sealants): Glass ionomers can release fluoride over time, supporting a fluoride release mechanism that can help with long-term decay prevention in certain situations.
Your dentist may describe these as Pit and Fissure Sealants, with selection based on moisture control, eruption status, and caries risk.
How are dental sealants applied?
A typical dental sealant process takes only minutes per tooth. Cleveland Clinic outlines a straightforward sequence that matches common Dentistry workflows: clean, isolate and dry, etch, rinse and dry, place sealant, then cure it with a light.
A practical step-by-step view:
- Clean the tooth to remove plaque, food, and debris.
- Keep the enamel dry (cotton or isolation).
- Apply an etching solution to improve bonding.
- Rinse and dry again.
- Paint the sealant material into pits and fissures.
- Cure with a light so the sealant hardens.
This is a preventive dental treatment, not a filling. No drilling is involved for routine sealants.
What do sealants feel like and what do sealants look like?
Most people feel no pain. Some people notice a slight “high spot” at first. If the bite feels off after placement, a dentist can adjust the surface so chewing surfaces feel normal.
Risks / Benefits
What are the benefits of dental sealants?
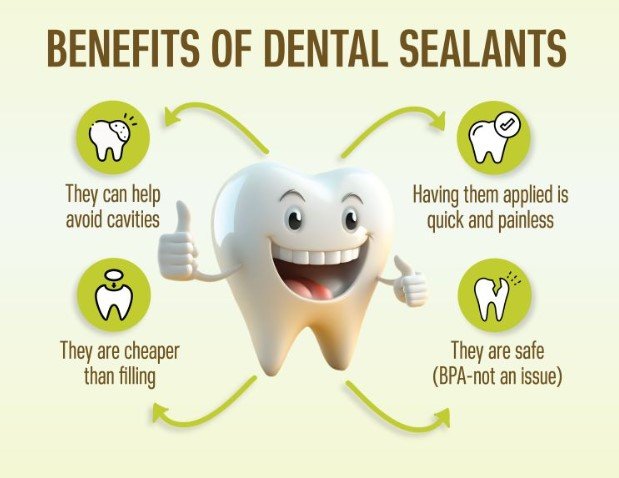
Dental sealants benefits are direct and measurable for many patients:
- Reduce your risk of tooth decay on chewing surfaces. The CDC describes sealants as preventing a large share of cavities in back teeth.
- Seal hard-to-clean anatomy. Brushing and flossing miss some pits and fissures, so sealing out plaque and food particles helps.
- Cost-effective cavity prevention. Preventing a cavity often costs less than repairing one with restorative dentistry.
- Posterior teeth safeguard. Sealants focus protection where decay frequently starts in children and adolescents, supporting childhood decay control.
Are dental sealants safe and effective?
Dental sealants are widely used and considered safe and effective in routine care when placed correctly and checked at follow-up visits.
Bisphenol A (BPA) and sealants
Some patients ask about Bisphenol A (BPA). MouthHealthy (American Dental Association (ADA) consumer resource) states sealants may have a tiny amount of BPA and describes the exposure as not expected to cause harm at that level. Patients with questions should discuss material choices and allergy history with a dentist.
Are there disadvantages or risks?
Risks are real, but usually manageable:
- Sealants can wear, chip, or fall off. Mechanical wear protection is not permanent. Cleveland Clinic notes sealants often last up to about five years, so periodic checks matter.
- Trapped decay risk if placement is poor. If moisture control is inadequate, a sealant can fail or seal in bacteria. Proper technique and routine checks reduce this risk.
- Allergies are possible. MouthHealthy notes side effects are uncommon except in cases of allergy. Share allergy history with the doctor and care team.
Who Should Get Dental Sealants?
Dental sealants for kids and adolescents

Children and adolescents are common candidates. Cleveland Clinic describes timing as soon as permanent molars and permanent premolars erupt, to protect enamel during cavity-prone years. Sealants support tooth morphology protection during the period when oral hygiene habits are still developing.
Cleveland Clinic also reports that in the U.S., a large share of children and adolescents have sealants on permanent teeth, which reflects how routine the treatment is.
Dental sealants for adults
Sealants are not only for kids. Adults without existing fillings, crowns, or active decay on those chewing surfaces can benefit, especially with:
- High caries risk history
- Deep grooves
- Orthodontic appliances that complicate oral hygiene
- Diet patterns that increase exposure to sugars and fermentable carbohydrates
A dentist may recommend sealants as part of a broader Tooth Decay Prevention plan.
Sealants on baby teeth
Primary teeth (baby teeth) sometimes qualify when deep pits and fissures exist and the child has high decay risk. Keeping baby teeth healthy supports spacing for adult teeth and supports normal chewing and speech development.
Recovery and Outlook

What is the recovery time?
There is no downtime after dental sealants. People typically return to school or work right away.
When can you eat or drink?
Most patients can eat and drink right after the appointment. Extremely hard, sticky, or chewy foods can chip or erode sealants, so moderation helps with longevity.
How long do tooth sealants last?
Cleveland Clinic describes sealants lasting up to about five years, with replacement as needed. MouthHealthy also notes sealants often last several years and should be checked at routine visits.
Dental Hygiene After Sealants
Sealants protect your teeth, but they do not replace oral hygiene. A complete Dental Hygiene plan still needs:
- Brushing twice daily with fluoride toothpaste (Fluoride supports enamel strength).
- Flossing daily to remove plaque between teeth and near gums.
- Regular professional cleanings so hygienists can remove hardened plaque and check sealant edges.
Sealants reduce risk, but cavities can still form on unsealed surfaces or at the margins if plaque control is poor.
When To Call the Doctor

Call a dentist or schedule a visit if any of these occur:
- A rough edge, crack, or missing sealant. A broken barrier can raise decay risk.
- New tooth sensitivity on a sealed molar or premolar. Sensitivity can signal bite issues, wear, or early decay elsewhere.
- Persistent toothache, gum swelling, or signs of infection. Sealants are preventive, not a treatment for pain that already suggests deeper disease.
- Concerns about materials or allergies. Ask about resin-based sealants vs glass ionomer sealants if allergies or sensitivities exist.
Additional Details
Are dental sealants necessary?
The practical answer is: sealants are often a smart choice when deep grooves and caries risk exist, but sealants are not for every tooth. Cleveland Clinic notes sealants are not placed on teeth with existing fillings or crowns, and partially erupted teeth may not benefit until eruption is complete.
Why do dental sealants fail?
Dental sealants fail for predictable reasons:
- Moisture contamination during placement reduces bonding strength.
- Heavy chewing forces or bruxism can accelerate wear.
- Frequent hard or sticky foods can chip the coating.
- No follow-up checks allow small failures to progress unnoticed.
Do sealants prevent cavities completely?
Sealants lower risk, mainly on chewing surfaces. Cavities can still develop:
- Between teeth where flossing matters
- Along the gumline where plaque collects
- Under a failed sealant if it breaks and decay is not addressed
Conclusion
Dental sealants protect your teeth by sealing out cavity-causing bacteria and food debris from deep grooves on the chewing surfaces of back teeth molars and premolars, reducing tooth decay cavities as part of preventive dentistry treatments. The best results come from the full routine: sealants placed well, checked at follow-ups, paired with fluoride, brushing, flossing, and consistent Dental Care visits.
