Seeing blood in the sink after brushing or flossing is a common experience, but it is never normal. Bleeding gums are a critical warning sign from your body, indicating inflammation and often the onset of periodontal disease. Ignoring this symptom is a mistake, as chronic inflammation in the gingival tissue is the primary precursor to gum recession and eventual alveolar bone loss.
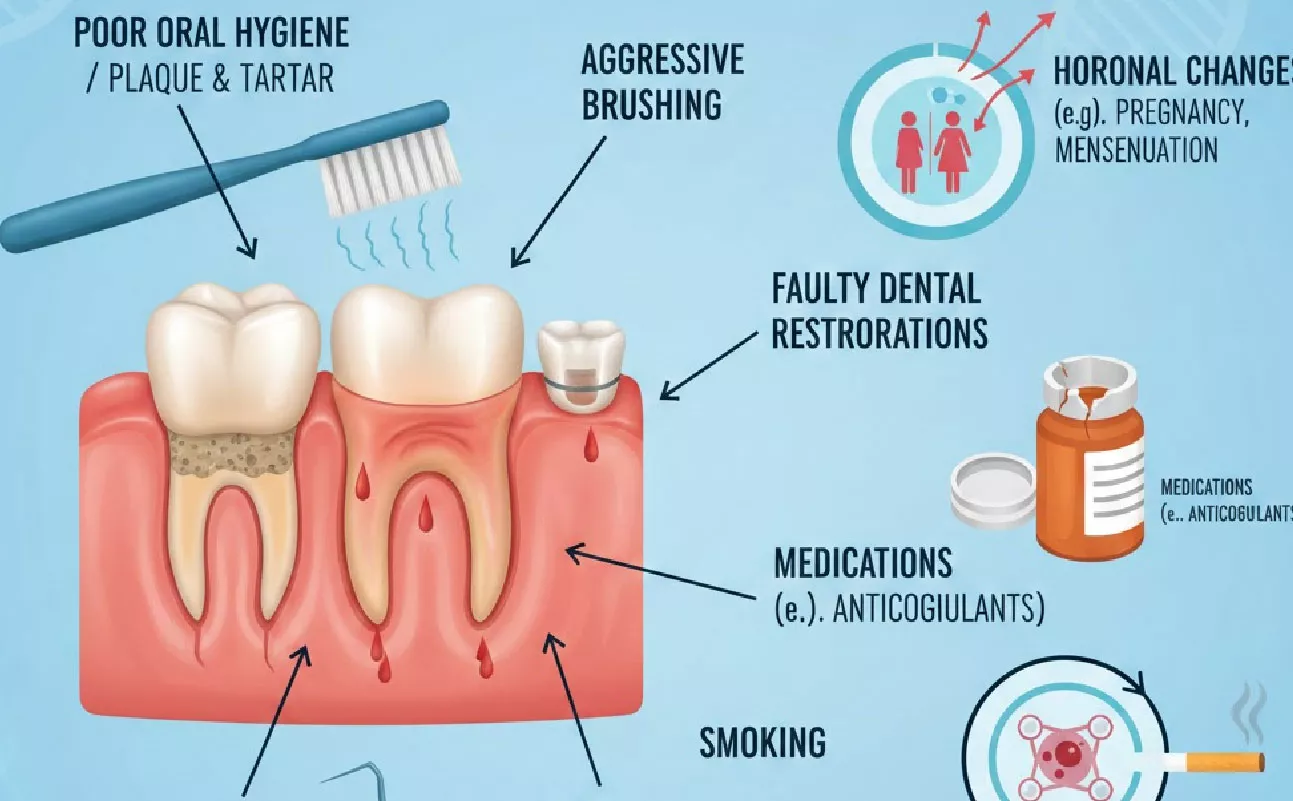
While occasional bleeding might be due to a new, aggressive brushing technique, persistent bleeding is almost always a sign that the delicate balance of your oral microbiome has been disrupted. This guide delves into the seven primary causes of bleeding gums, explaining the underlying biological mechanisms and the necessary steps to address them before they lead to more severe conditions like periodontitis.
1. Plaque Accumulation and Gingivitis (The Most Common Cause)
The overwhelming majority of bleeding gums cases are caused by the accumulation of dental plaque along the gingival margin (where the gum meets the tooth).
Mechanism:
- Plaque Biofilm: When plaque—a sticky, colorless film of bacteria—is not removed effectively by brushing and flossing, the bacteria release toxins.
- Immune Response: These toxins trigger an immune response in the gingival tissue. The body increases blood flow to the area to deliver immune cells, causing the gums to become red, swollen, and tender.
- Gingivitis: This initial stage of inflammation is called gingivitis. The increased blood flow makes the gum tissue fragile, and even light contact from a toothbrush or floss can cause it to bleed easily.
Gingivitis is reversible. However, if left untreated, the chronic inflammation progresses deeper, leading to the destruction of the periodontal ligament and alveolar bone, which is the hallmark of periodontitis and the direct cause of gum recession.
2. Progression to Periodontitis (The Severe Stage)
If gingivitis is not reversed, it progresses to periodontitis. This is a destructive, chronic inflammatory disease that affects the supporting structures of the teeth.
Mechanism:
- Pocket Formation: The chronic inflammation causes the gingival tissue to pull away from the tooth, creating periodontal pockets.
- Bone Loss: Bacteria colonize these deep pockets, and the body’s immune response begins to destroy the alveolar bone that anchors the teeth.
- Severe Bleeding: Bleeding becomes more frequent and often occurs spontaneously or upon slight probing, indicating active tissue destruction.
Periodontitis is the most significant pathological cause of gum recession. As the bone is lost, the gum tissue follows, exposing the sensitive tooth root and leading to tooth mobility and eventual loss.
3. Aggressive Brushing and Mechanical Trauma

Paradoxically, attempting to clean too vigorously can also cause bleeding gums. This is a form of mechanical trauma.
Mechanism:
- Force: Using a hard-bristled toothbrush or applying excessive force (horizontal scrubbing) physically damages the delicate gingival tissue.
- Abrasion: This trauma causes micro-lacerations and bleeding, and over time, leads to gingival abrasion and mechanical recession.
Solution: Switching to a soft-bristled toothbrush and adopting the Modified Bass Technique (gentle, circular motions angled at 45 degrees) is essential to remove plaque without causing trauma.
4. Hormonal Fluctuations (Systemic Factors)
Hormonal changes can significantly increase the sensitivity and inflammatory response of the gums, even with minimal plaque present.
Key Periods:
- Pregnancy: Elevated levels of progesterone and estrogen increase blood flow to the gums, making them more susceptible to inflammation and bleeding (pregnancy gingivitis).
- Puberty and Menstruation: Similar hormonal surges can cause temporary gum sensitivity and bleeding.
- Menopause: Reduced estrogen levels can lead to dry mouth (xerostomia) and increased susceptibility to inflammation.
These hormonal changes do not cause periodontal disease, but they exaggerate the body’s response to the existing plaque biofilm, making effective oral hygiene even more critical during these times.
5. Certain Medications and Systemic Diseases
Several systemic factors can compromise the body’s ability to maintain healthy gums, leading to increased bleeding.
| Systemic Factor | Mechanism Affecting Gums | Semantic Entity |
| Blood Thinners | Medications like aspirin or anticoagulants reduce the blood’s clotting ability. | Coagulation Disorder |
| Diabetes Mellitus | Impairs the immune system and reduces blood flow, making the body highly susceptible to infection and chronic inflammation. | Impaired Immune Response |
| Vitamin Deficiencies | Lack of Vitamin C (scurvy) or Vitamin K (clotting) weakens capillaries and impairs healing. | Nutritional Deficiency |
| Immunosuppressants | Medications used for organ transplants or autoimmune diseases reduce the body’s ability to fight infection. | Compromised Immunity |
Systemic diseases like uncontrolled Diabetes Mellitus accelerate the progression of periodontitis and the resulting alveolar bone loss, making gum recession more rapid and severe.
6. Poor Nutrition and Diet
A diet high in cariogenic carbohydrates and low in essential vitamins fuels the problem from two angles:
- Bacterial Fuel: Sugars feed the pathogenic bacteria in the plaque biofilm, increasing toxin production.
- Structural Weakness: Lack of Vitamin C impairs collagen synthesis, weakening the structural integrity of the gingival tissue and making it prone to bleeding and breakdown.
Solution: A diet rich in anti-inflammatory foods (Omega-3s, polyphenols) and structural nutrients (Vitamin C, Vitamin D, Calcium) supports the body’s natural healing processes and reduces the systemic inflammatory load.
7. Ill-Fitting Dental Appliances and Restorations
Dental work that is poorly fitted can create areas where plaque is impossible to remove, leading to localized inflammation and bleeding.
Examples:
- Overhanging Fillings: A filling that extends beyond the natural tooth contour creates a plaque trap.
- Ill-Fitting Crowns or Bridges: Gaps or rough edges near the gum line harbor bacteria.
- Loose Dentures or Orthodontic Appliances: These can rub and irritate the gingival tissue, causing chronic inflammation and bleeding.
These issues create localized plaque retention factors that accelerate the inflammatory process in a specific area, often leading to localized gum recession on the affected tooth.
The Critical Connection: Bleeding Gums and Gum Recession

It is crucial to understand that bleeding gums are not just a nuisance; they are the earliest stage of the inflammatory process that, if left unchecked, leads directly to gum recession.
Gingivitis (bleeding gums) → Periodontitis (deep pockets, bone loss) → Gum Recession (exposed root, sensitivity).
By addressing the cause of the bleeding immediately, you are taking the most effective step to prevent the destructive cascade that results in permanent tissue loss.
Targeted Treatment for Bleeding Gums
The first step in treating bleeding gums is always professional cleaning to remove hardened plaque (calculus) and a commitment to meticulous home care.
For targeted home treatment, reducing the pathogenic bacterial load is paramount. Products that deliver potent, natural antibacterial agents directly to the gingival margin and into the gingival sulcus can significantly accelerate the reversal of gingivitis.
Nature’s Smile Gum Balm, for example, utilizes a concentrated blend of natural extracts known for their anti-inflammatory and antibacterial properties. By applying such a formula directly to the inflamed tissue, you are:
- Reducing Inflammation: Calming the immune response that causes the bleeding.
- Killing Pathogens: Targeting the bacteria that release the toxins.
- Supporting Tissue: Creating an environment conducive to the healing of the gingival tissue.
This targeted approach, combined with proper brushing and flossing techniques (gentle, non-traumatic), is the most effective way to stop the bleeding and prevent the progression to periodontitis and gum recession.
External Links
- American Dental Association: Gum Disease
- National Institute of Dental and Craniofacial Research: Periodontal Disease
- Mayo Clinic: Bleeding Gums
- Journal of Periodontology: Systemic Factors in Periodontitis
Call-to-Action
Don’t ignore bleeding gums—it’s your body’s warning sign. Address the inflammation and bacterial load immediately. For targeted support against the pathogens that cause bleeding and recession, integrate Nature’s Smile Gum Balm into your daily care.